Helene Castel
University of Rouen, France
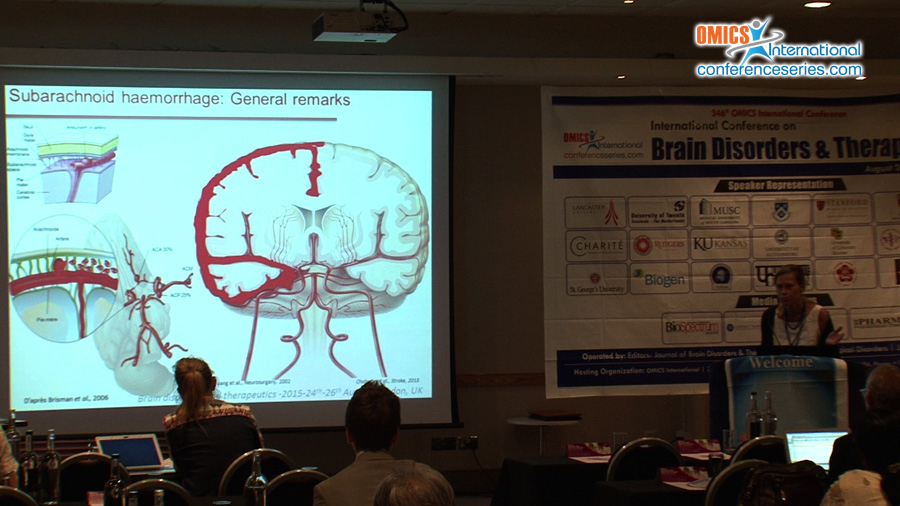
Title: Characterization of a mouse model of subarachnoid haemorrhage. Involvement of the urotensin II peptide system on vasospasm and neurosensitivomotor deficits
Biography
Biography: Helene Castel
Abstract
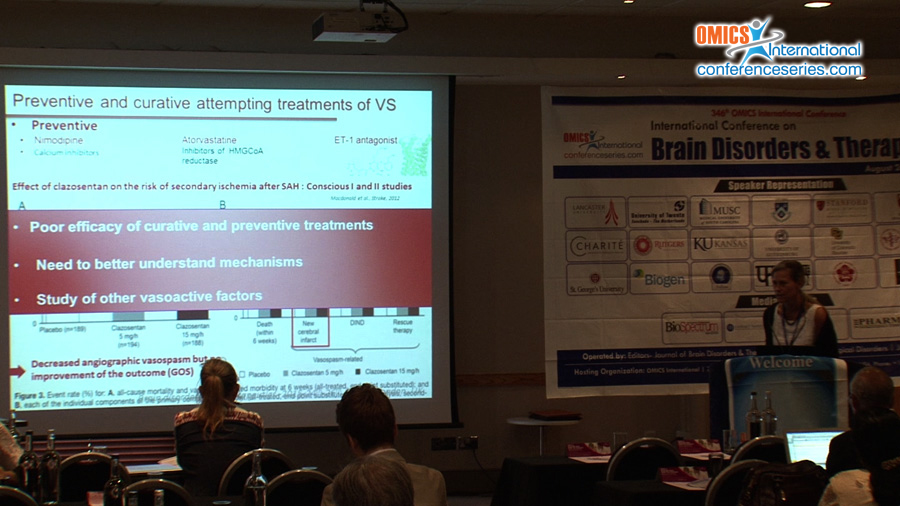
Subarachnoid haemorrhage (SAH) refers to extravasation of blood into the compartment between the brain and the tissue that covers the brain. This is often due to a ruptured aneurysm and accounts for up to 5% of all new stroke cases. Survivors of SAH commonly experience sequels that affect their day-to-day lives and which could persist years after; these include fatigue, memory deficits, executive function, language, depression and sleep disorders. The cerebral arterial vasospasm (CV) is a complication of the SAH, and may by associated with neurological deficits, microthrombosis and cerebral ischemia. Despite advances in diagnosis and surgical treatment, effective therapies are still limited and clinical outcomes remain disappointing. The CV may be due to vasoactive peptides which are released locally and which, under normal conditions, control the blood/brain exchange. One of the most potent vasoactive peptides is urotensin II (UII). Urotensin II (UII) and its paralog URP activate a G protein coupled receptor (GPCR) named UT. UII exerts a wide range of physiological effects and regulate the endocrine, cardiovascular, kidney and immune functions. Our study aimed at providing significant advances and proof of concept of a new therapeutic target in SAH in a major area of public health involving neurological disability and the dramatic change in the quality of life. We led a single-center prospective study over a period of 24 months, including all patients with SAH of aneurysmal origin with external ventricular bypass and aneurysm exclusion, classified stage 1 or 2 in the WFNS scale. Blood and CSF samples were collected from D0 to D8. The ROC curve showed that the plasma concentration of UII is a discriminating factor for the occurrence of CV (AUC 0.824, P = 0.02, patent FR1356995, 2013). A mouse model of SAH was also developed via a double injection of arterial blood into the magna cisterna during two consecutive days. Occurrence of CV of the cerebral middle, basilar and anterior arteries and a number deposition of fibrin (microthrombis) were observed from the 2nd to the 14th day post-SAH, as well as increase in the activity of caspase-3 from Day 3 to 14 in brain cortex, hippocampus, endothelium and choroid plexus. Impaired sensorimotor functions (beam walking test) were detected from D7 to D10. Then, we investigated the impact of the UII system in this SAH model my means of wild-type (UT+/+) and KO-UT (UT-/-) mice. UT-/- mice do not exhibit any remarkable phenotype. The β-galactosidase activity (reporter of the UT transcription) was very faint in the brain cortex, endothelium, and choroid plexus in Sham UT-/- mice and strong in brain cortex, hippocampus, choroid plexus and microvessels 10 days post-SAH. Consistent with these observations, we demonstrated the expression of UII peptide in the brain cortex, the hippocampus and in some large and small arteries only in SAH mice. Interestingly, the UT ligand urantide, listed so far as \"antagonist\", but now definitively characterized as a biased ligand1, completely prevented CV, microthrombosis and consecutive neurosensitivomotor deficits in SAH mice, suggesting that UT ligands may constitute interesting therapeutic tools. We should in the future, explore the effect of other UT biased ligands which may cross the blood brain barrier and bind UT, mainly expressed during the course of the SAH pathology. These compounds with minimal side effects can be extremely innovative in the treatment of SAH, but also in other cardiovascular pathologies.